Digital transformation for resilience and better health and social care

Chief Digital Information Officer (CDIO) in the Department of Health, Dan West, outlines six opportunities to create more sustainable and resilient health and care services through digital.
West explains that the pandemic has dominated much of the landscape of health and care service delivery over the past two years, with the nature of Covid-19 driving a significant demand for digital services. However, alongside the many challenges that have been put to digital delivery of services, opportunities have also emerged to build a better and more resilient health and care system through transformation.
In setting out his identified six areas of opportunity, West says that it is important to first acknowledge the context of the nature of the challenge being faced in health and social care in Northern Ireland, adding weight to the importance of digital opportunity.
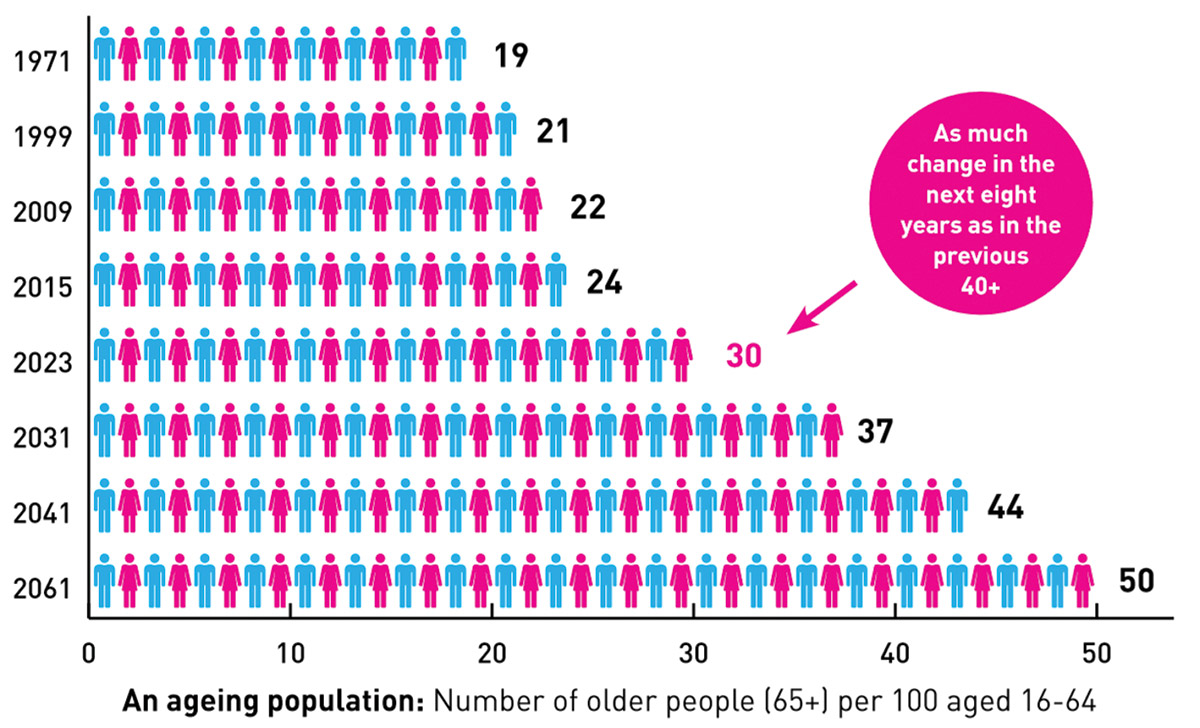
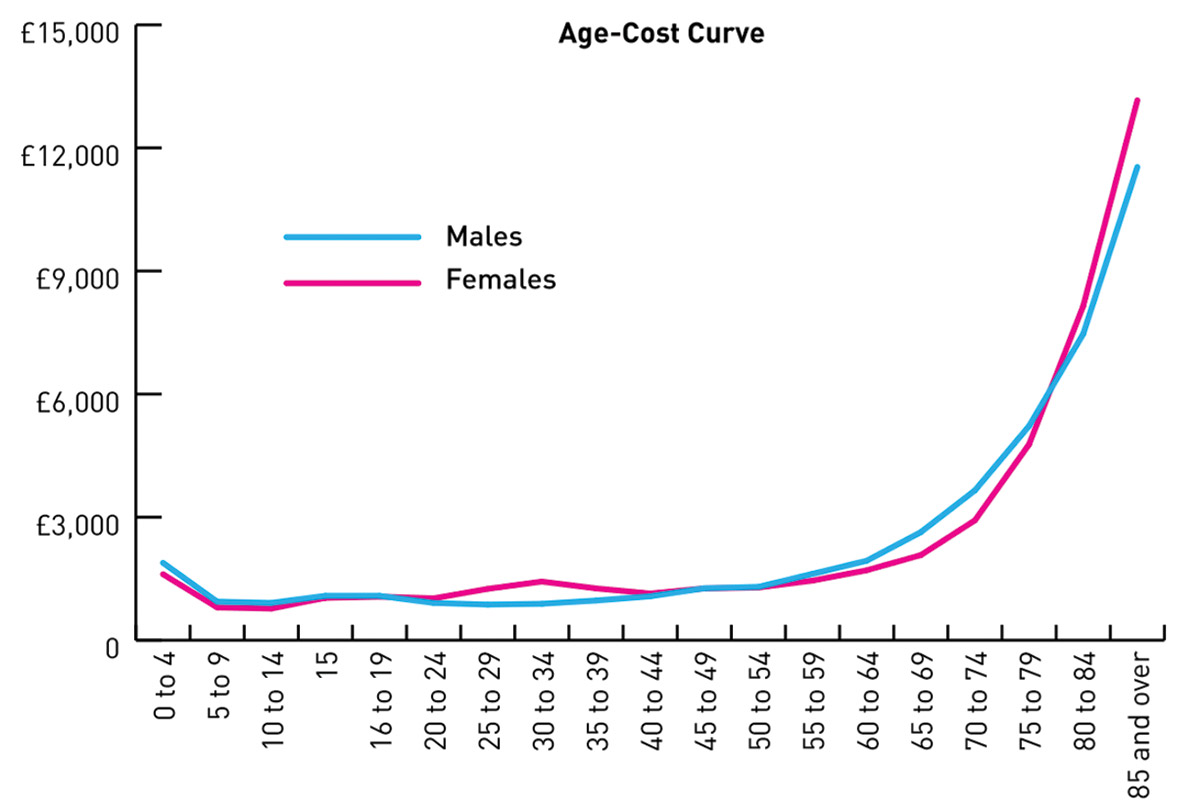
Northern Ireland’s demographics is changing rapidly and by 2030, the number of people aged over 65 is expected to be double what it was in the year 2000. This is significant when considering that citizens over the age of 65 currently account for more than 40 per cent of all health and social care spending, despite only making up 14 per cent of the population share.
Added to this is the fact that current health trends estimate that by the age of 70, 80 per cent of the current population will have one or more chronic conditions. By the age of 80, 60 per cent of the population will have three comorbidities or chronic conditions. Whilst overall people are living longer in Northern Ireland, a significant deprivation gap exists in relation to life expectancy. The life expectancy for males in Northern Ireland’s most deprived areas is on average some seven-and-a-half years less that their counterparts in the least deprived areas.
Finally, changing demographics is having a significant impact on demand. For example, between 2009 and 2014, demand for access to GP surgeries increased by over 20 per cent. Northern Ireland’s average of seven consultations per patient per year is one of the highest of any OECD countries. For context, in the Republic of Ireland the average is three per year. That the health and social care system is not coping well with increased demand can be observed in large increases in outpatient, inpatient and day case waiting lists.
West believes there are six things the Department can and is doing to build a more sustainable and resilient service through digital.
Firstly, he highlights in the need to break the current linear relationship between the demand for services and the capacity to deliver those services. Pointing to the rapid uptake of digital services such as the StopCOVIDNI proximity app and use of digital vaccination appointment booking as evidence that citizens in Northern Ireland want to be more empowered and to become active partners in their healthcare journey, digitally, he says that digital tools have the potential to increase self-service, ultimately improving citizen experiences and conveniences.
He believes that providing patients and carers with greater visibility and control over their treatment and care pathways through digital can break the current linear relationship between demand and capacity. With Northern Ireland behind the curve in this regard, when compared to the rest of the UK, West says that this approach sets out a focus for digital health transformation in the coming years.
“The Prime Minister’s announcement on working from home in 2020 flipped a switch that made an existing demand for transformation necessary overnight.”
Secondly, West identifies a need to shift towards a more standardised and evidence-based care model across Northern Ireland’s health and care provider organisations, putting safety and quality at the heart of all new processes and systems. West says that work is already underway in this regard and points to examples of major programmes such as the Digital Identity Service, the new electronic patient record system announced in 2020, and the Northern Ireland picture archive and communications system + solution (NIPACS+), a single system with the facility to store, distribute, view, and diagnose images by all organisations involved in the delivery of care.
Thirdly, West says that health and social care service must get better at joining up services and information across the sector and protecting the information as it is used. The CDIO points to ontology, integration, cybersecurity, and information governance as areas in need of greater consideration if opportunities for better service delivery through digital are to be taken up.
The fourth opportunity for digital West identifies is the support of staff to do their work more easily, efficiently, and collaboratively in multidisciplinary multi-organisation teams. “As a technologist, we have known that this journey, to create mobile, flexible tools to enable our staff to maximise their efficiency, is one we have needed to take for a long time,” he says. “The Prime Minister’s announcement on working from home in 2020 flipped a switch that made an existing demand for transformation necessary overnight. The programmes we are delivering in health and social care are many and varied but the Digital Workplace Programme (DWP), the Equip programme and HSC digital are some examples of how we are developing the services through digital.”
“Health and social care is a sector built on innovation, but the reality is that despite all of that amazing innovation which happens across health and social care every day, not much of it has an impact at scale on the bottom line of economic sustainability of health and care.”
West’s fifth point relates to the better use of data, specifically, to understand the population and their needs and ultimately, to improve how information is connected and used to create insights and develop services. The CDIO points to the creation of a new health and social care strategy, likely to point to the need for a new social care information institute, with the aim of delivering:
- education and evangelism;
- training and skills development;
- data platform infrastructure development and delivery;
- analytics and insight Centre of Excellence; and
- legal and information governance.
Finally, West says that better legal and information governance can enable opportunities for better work within the innovation eco-system within and outside health and social care to create real impact at scale, from advancements in research and emerging technologies. “Health and social care is a sector built on innovation, but the reality is that despite all of that amazing innovation which happens across health and social care every day, not much of it has an impact at scale on the bottom line of economic sustainability of health and care,” says the CDIO. “Northern Ireland has the highest age adjusted per capita cost in the UK and among the worst waiting lists for elective and day case services in Europe, so how do we develop a new innovation strategy that has that bigger impact and alignment between innovation and the big challenges we face as a service?”
Concluding West says that the development of a new innovation strategy is underway, with four key components:
- a new digital innovation pathway that assesses technology readiness levels to determine which technologies and initiatives are ready to scale;
- a digital innovation infrastructure to facilitate, scale up and spread of those successful innovations;
- an innovation support hub to support and optimise the use of digital and data to support innovation and a new governance structure that helps to align innovation to executive level initiatives and stakeholders; and
- governing innovation.