Addressing mental ill health: The rise of antidepressants

SDLP MLA and Vice-Chair of the All-Party Group on Mental Health, Mark Durkan talks to David Whelan about the findings of his recently commissioned research in to mental health services and the treatment of depression in Northern Ireland.
Describing the findings of a Northern Ireland Assembly research paper, Mental Health Services in Northern Ireland, authored by Grainne Crealey as “a catalogue of chaos”, the Foyle MLA states bluntly his opinion that when it comes to health services in Northern Ireland “the only consistency is in missed opportunities, failure to implement expert recommendations, and the chronic underfunding of mental health services”.
Durkan was speaking following receipt of a briefing paper report he commissioned which looked at comparing the costs of antidepressant prescribing and talking therapies in the treatment of depression in the region.
Approximately one-in-five of Northern Ireland’s population were recorded as receiving antidepressant medication during 2020/21, equating to almost 24 per cent of females and 14 per cent of males.
The Mental Health Foundation recently estimated that experiences of mental health problems in Northern Ireland are some 25 per cent above rates in England, and depression levels are the highest of any region of the UK.
Offering an overview of mental health in Northern Ireland, based on the report’s findings, Durkan says: “The prevalence and severity of mental health problems are higher than the rest of the UK, an arguably unavoidable fact given the legacy of conflict and globally we have the highest rates of PTSD [according to a 2011 study undertaken by Ulster University].
“The report further evidences that poor mental health affects huge swathes of the population with high levels of referrals for children, adolescent, and maternal mental health services. Given this landscape, it is staggering that the allocation for mental health represents just 5.7 per cent of the health budget. In comparison, NHS England spend 14.1 per cent of their overall health budget on mental health services.”
Describing the rise in antidepressant prescription costs and usage as “alarming”, the Vice-Chair of the All-Party Group on Mental Health suggests that the finding that one-fifth of the population are taking antidepressant medication could be attributable to “the dearth” of talking therapies and shortage of skilled health staff.
Findings in the briefing paper report are that antidepressant medication is now the most prevalent treatment for depression in Northern Ireland, GPs in Northern Ireland prescribe on average two-and-a-half times more antidepressants than their English counterparts and the region has the highest rate of repeat prescribing for antidepressants among the four UK jurisdictions.
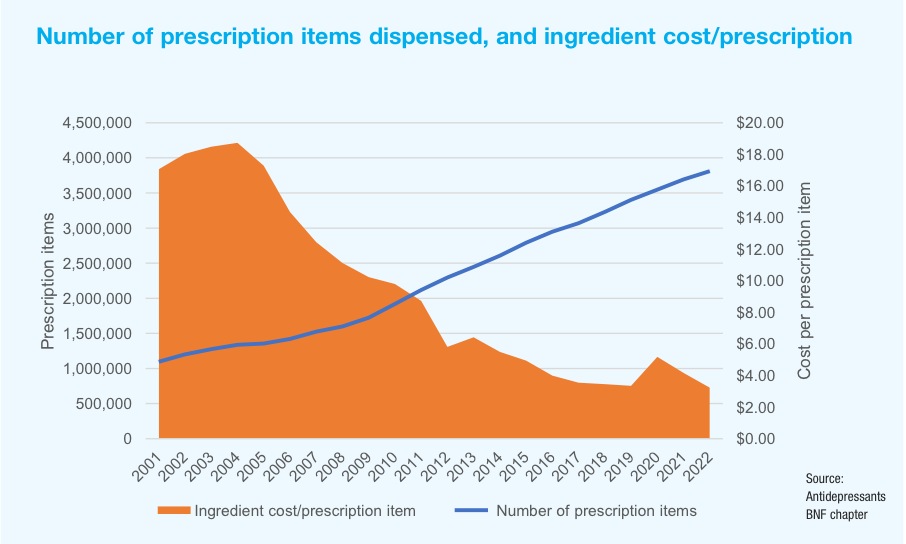
Despite an increase in the number of prescription items dispensed, the cost of prescribing antidepressants has reduced significantly, almost halving in the past 20 years.
Psychological therapies have been demonstrated to be equally as effective as antidepressant medication and are recommended by the National Institute for Health and Care Excellence (NICE) for the treatment of depression. However, waiting lists for talking therapies continue to grow.
On 30 June 2023, there were 2,251 total waits for a Child and Adolescent Mental Health Service (CAMHS) assessment in Northern Ireland, of which more than half (1,205) were waiting more than the targeted nine weeks.
Research studies suggest that talking therapies can lead to cost savings by reducing the need for more expensive treatments, such as medication and hospitalisations. They can also improve work productivity and reduce healthcare utilisation.
However, recently, the NIAO report was critical of the lack of regional standardisation and a fragmented information technology infrastructure in relation to mental health services provision across Northern Ireland, concluding that it was unable to say assess whether money being spent represents value for money.
Postcode lottery
Approximately 68 per cent of GP surgeries in Northern Ireland offered a counselling service in 2020/2021, notably however, provision varies depending on location, and there are disparities in service availability amongst the various health trust areas.
Calling for the creation of new care pathways and the expansion of talking therapies, Durkan says: “The ‘postcode lottery’ associated with these type of services is notorious, and it is difficult to comprehend why areas like Derry and Strabane, which has among the highest levels of mental illness, has the lowest access to psychological therapies. Research generally highlights that psychotherapy and methods like cognitive behavioural therapy (CBT) are highly effective and can reduce the need for medication and hospitalisations.”
Durkan suggests that resources to address Northern Ireland’s growing mental health crisis and improve service provision be properly ring-fenced.
“We have seen that monies previously earmarked to improve mental health pathways as part of the confidence and supply agreement of 2018 were diverted to plug funding gaps in front line services.
“I have written to the Department of Health asking for assurances that the £2.5 million earmarked for the Mental Health Strategy for 2021/22 was used to develop specific outcomes. The reality is that this life-saving strategy cannot be delivered in the absence of an Executive but confirmation that a solid foundation of work was achieved as part of that allocation would provide some degree of comfort.”
The 10-year Mental Health Strategy published in June 2021 was accompanied by a funding plan which outlined an implementation cost of £1.2 billion over a decade. However, no such funding has been agreed in the absence of an Executive or a multiyear budget.
“It is estimated that mental health problems cost the Northern Ireland economy £3.4 billion a year,” explains Durkan. “The failure to properly resource these services will result in colossal costs for society, for the health service and most importantly, for people.
“The North is caught in a vicious cycle of ever-increasing demand for services and a steady depletion of resources. Mental health services are being pummelled from all sides; the inability to allocate the necessary funding within the department has been compounded by the cuts in primary school counselling provision and huge losses from European funding.
“Community-based services, which are lifelines for service users, are being financially squeezed, and the devastating impacts of this deepens the gap in mental health services.”
Durkan says that proper investment and the implementation of the Mental Health Strategy is key to addressing the crisis across communities.
“Enhanced collaboration is key to effective care and support. This strategy would help bring order to the chaos and disjointed nature of mental health services. It would ensure the many dedicated organisations working hard every day to help people, to change lives and to save lives, are properly supported.
“It is one thing to encourage people suffering from mental illness to seek support but quite another to ensure that access to effective and early support is readily available. We need the DUP to end their boycott of our institutions, to allow MLAs to get back to work and prevent Northern Irelands’s mental health crisis becoming a Pandora’s Box that cannot be curtailed,” he concludes.