Transforming the future of health and social care

Chief Digital Information Officer at the Department of Health, Dan West, discusses the current and future benefits of ongoing digital transformation in the health and social care sector.
Outlining the vision of the Department of Health’s 2022 Digital Strategy to deliver, before the end of the decade, the transformation of health and social care into a highly integrated and personalised system, with services tailored to an individual’s genetics, being data driven, and optimised by advancements in digital technology, West is quick to point out an existing projection that, without successful interventions, by 2040 the entirety of Northern Ireland’s block grant would need to be dedicated to health and social care services, due to the current trajectory of healthcare inflation.
“It is a stark figure and driving the digital transformation of health and social care in that financial context is not straightforward,” he explains.
The Department of Health’s Digital Strategy, alongside underpinning data, cyber security, and innovation strategies, outlines the strategic intent to 2030 and represents a £1.3 billion investment portfolio. Outlined in the strategy is an overarching vision of “making lives better for the people of Northern Ireland, using digital to transform the way we deliver health, care and wellbeing services”.
Underpinning this vision, West explains, is a recognition that without transformation: “Our children will not be able to get health and care in the way we expect to get it, unless we do something bold and different in the way we deliver those services.
“We need to change experiences, both for staff who give the care, and for service users who receive the care, and we need to drive transformation in a very different way than we have done over the last few years. This strategy helps us to understand that,” he says.
Currently, says West, the Department is doing a lot of “programmatic delivery”, which he explains is aimed at addressing technical debt and historic underinvestment.
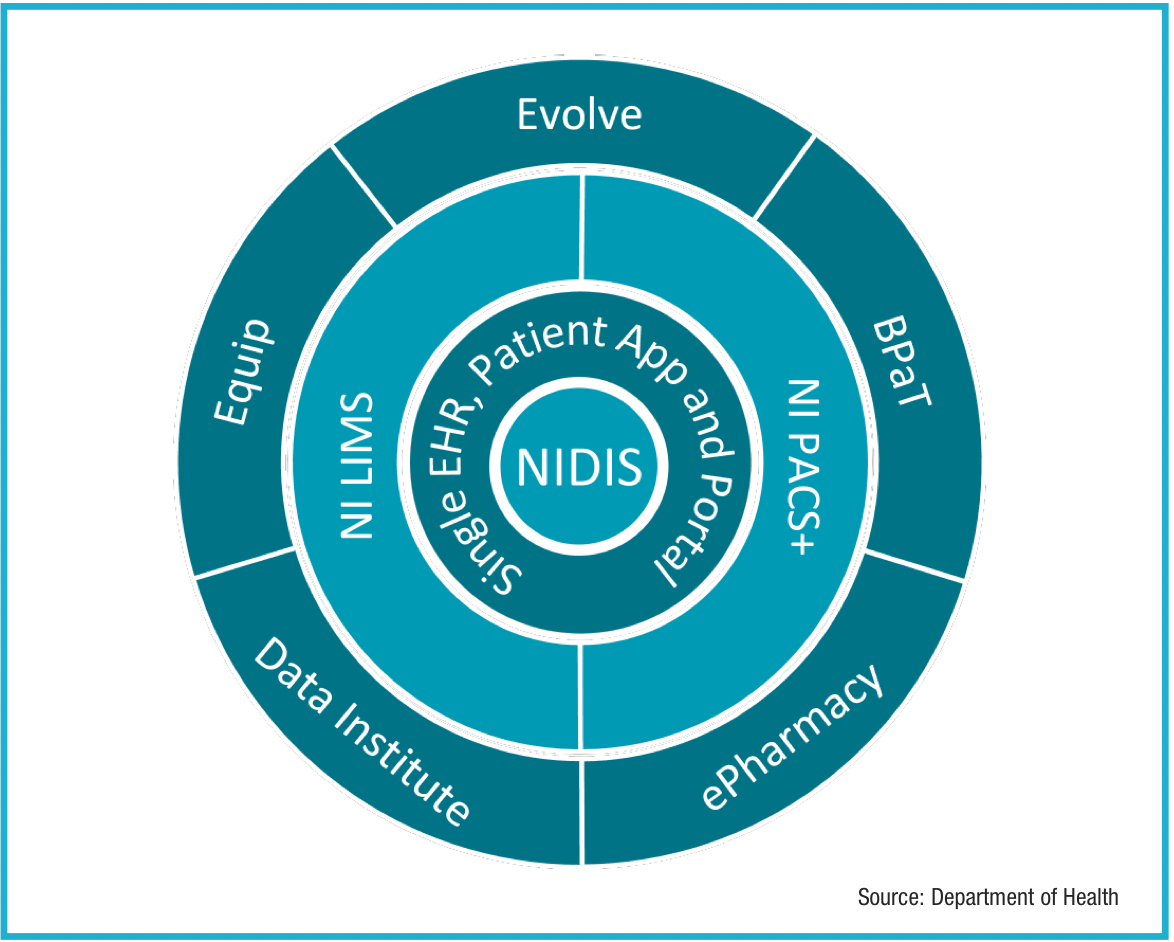
Offering a high level look at the investment portfolio, he points to the development of the ‘Encompass’ single electronic health record (EHR) being delivered on top of the Northern Ireland Digital Identity Service (NIDIS), both of which launched in 2023. This has enabled the ongoing rollout of converged clinical platforms, including Northen Ireland Laboratory Information Management System (LIMS) and the Northern Ireland Picture Archive and Communication System (NIPACS+), across secondary hospital care, mental health, community and social care services.
Wider again is the current delivery of some 80 projects in the enterprise portfolio delivery phase, with a further 80 in earlier stages of discovery, business case development, procurement or design – all aiming to improve care services and data capabilities. Included in the next wave of transformation are two investments that replace significant and outdated IT infrastructure and systems: the Northern Ireland Blood Production and Tracking project, to build a new vein to vein blood product tracking platform, and the Equip programme, which replaces current back-office systems with the new Oracle Cloud platform.
“Equip is a hugely impactful programme, and a really important next step for Northern Ireland – it will drive convergence and modernisation in our back office and provide a new technology platform for delivery of finance, procurement, logistics, HR and payroll”, explains West.
Highlighting recognition that much of the early work has been centred on technology, but that technology is not the end in itself, he stresses that improved services are about improved economic outcomes and improved health and social care for society.
“We need to pivot away from the big delivery activities of the last few years, and having broken the back of our technical debt, start thinking more about how we leverage the new platforms, build our capabilities to do transformation at the front line of service delivery, and make care better for people in this region.
“Building a new digital transformation and innovation capability collectively from the centre out to all of the care delivery organisations and care professionals is a large area of focus for my team currently.”
Reflecting on the successes of the last few years, West outlines what has been a busy implementation roadmap.
Since 2019, the Department has been developing a range of business cases, and working with stakeholders, particularly financial leaders with economic responsibility to approve the investment portfolio. While the outbreak of Covid-19 served to disrupt the planned digital journey, West explains that much progress was made on digital transformation during this time.
Pointing to the rollout of a completely new Microsoft environment, the CIO explains that this underpinned the convergence of clinical services and the enablement of remote working during the pandemic.
West goes on to explaining that by May 2025, the Department will have completed the roll out of Encompass, which will be “globally unique” as a single, national platform including both health and social care services being supported by a single system.
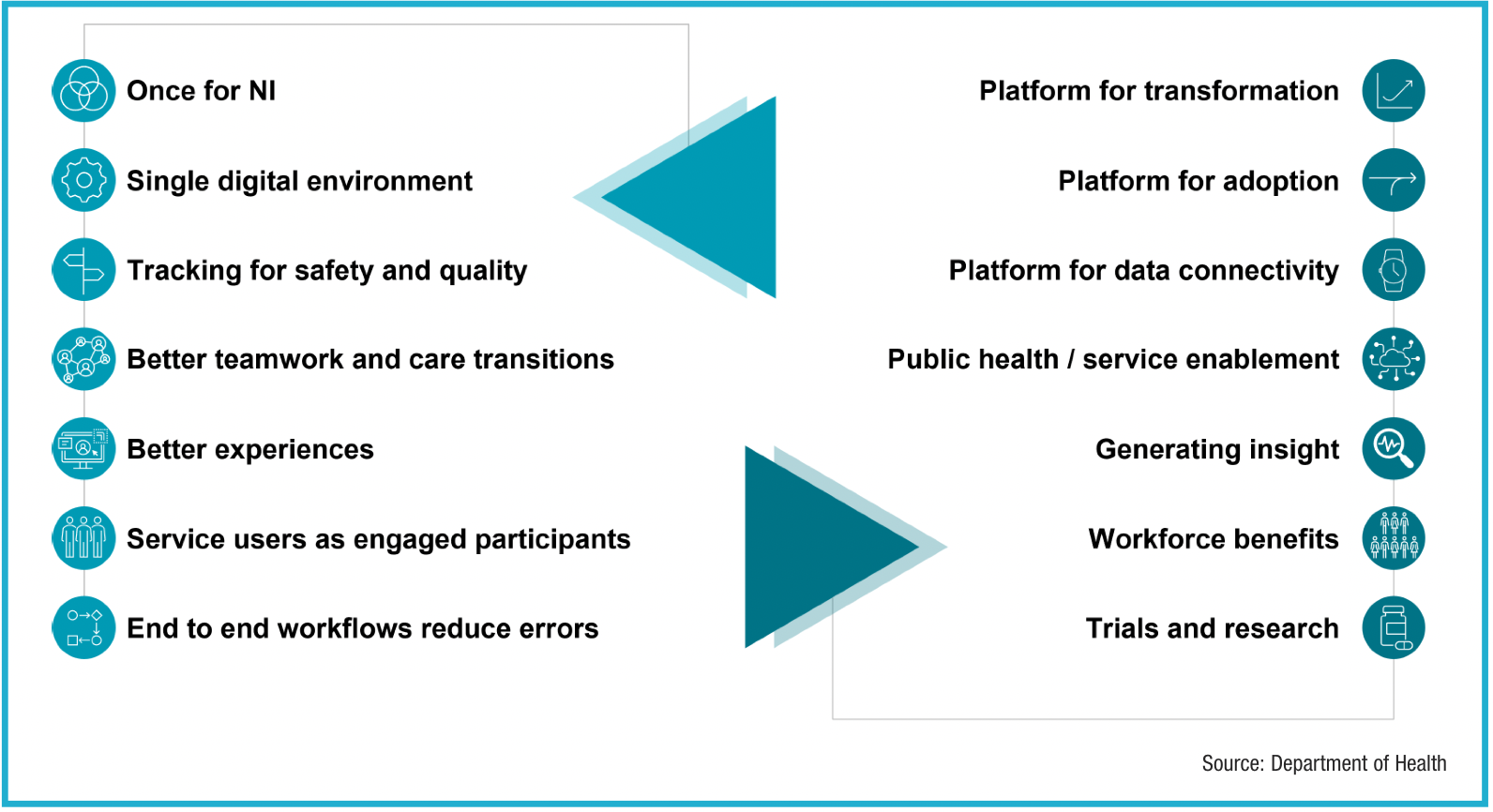
Discussing the impact of progress to date, West says: “‘Once of Northern Ireland’ should not be overlooked.
“The fact that we now have a single converged platform for all organisations and services in secondary care, mental health, community services, and social care, to deliver care models and care outcomes, is a huge accomplishment. Health and social care delivery is understandably complex, so the ability to simplify this by delivering a single platform brings a lot of benefits.
“The single digital environment brings all professions and services into one information environment, digitally enabling a range of workers who would not previously have had access to technology. We have rolled out masses of end user devices and end points to staff who otherwise would not have interacted with digital records as part of the way they do their jobs.
“A second advantage is the ability to track for safety and quality. We now have a single place to automate the movement of work around our system. Diagnostic tests in laboratories and in medical imaging currently move digitally through the system, based on the new platform. Now, we can bring diagnostic results into clinical workflows and provide protocolised alerts to clinicians involved in the care of an individual.”
Other benefits outlined by West include better teamwork and efficient care transitions; better service user experiences; service users as engaged participants; and the reduction of errors in end-to-end workflows.
Next steps
Returning to the vision of helping clinicians to transform the services they deliver, West recognises that between 80 to 90 per cent of all healthcare interactions occur in primary care, he says: “Having made some headway in digitising secondary care, we need to shift focus to think about how we are going to work with stakeholders to help transform primary care, including community pharmacies – there is huge benefit in working with GPs to continue to improve digital capabilities in practices and in how our GPs enable services for citizens.”
West reflects on the fact that the investments are not about digitising the current operations “What we have built and bought for ourselves is an ability to drive change in a very different way than we did before. Converged platform and converged capabilities allow us to influence change more easily than we were able to before.
“We have got better connectivity, and will be able to ingest a broader range of data sources, including wearables, in order to manage chronic diseases, without putting the burden onto clinicians for dealing with that data.”
Concluding, West says: “The goal is not the technology, the technology is a means to an end – the ultimate goal is improved care outcomes, better care experiences for service users and staff, and a more sustainable health and care economy for our children. Healthcare is not about technology, it is about people.”