Workforce pressures underpin GP ‘crises’

Efforts to increase the number of general practitioners in Northern Ireland are not having the desired effect, as fewer GP sessions are being delivered, a report has found.
Examining access to general practice in Northern Ireland, the Audit Office finds that despite a 9 per cent increase in the total number of GPs between 2018 and 2023, changing patterns of GP work has led to an overall decrease in whole-time equivalents, making it likely that fewer GP sessions are being delivered.
Despite efforts to grow the general practice workforce in recent years, including the establishment of a departmental working group in 2021/22 and an increase in training places from 65 to 121 over the decade from 2014, the report identifies a trend of increased training places being taken up by international medical graduates, who are deemed less likely to remain in Northern Ireland after completion.
The findings were part of a wider report detailing the “extreme pressure” facing GP practices in Northern Ireland, including that almost one-in-three GP practices has sought crisis support services in the last four years.
The Department of Health spends around £375 million per year on over 300 GP practices in Northern Ireland, which equates to roughly 5 per cent of the total health and social care budget.
GPs, under contract with the Department of Health, provide services as independent contractors and are a vital part of primary care delivery in Northern Ireland.
In total, 13 GP practices in Northern Ireland either handed back or gave notice to hand back their contracts in Northern Ireland in the year between March 2022 to March 2023. While alternative providers have been found for all of these practices, nine are on a temporary basis.
The potential for more practices to hand back their contracts is evident in the findings that in the past four years, 30 per cent (98 practices) have sought support from the General Practice Improvement and Crisis Response Team, which develops and implements recovery plans for practices identified as ‘at risk’.
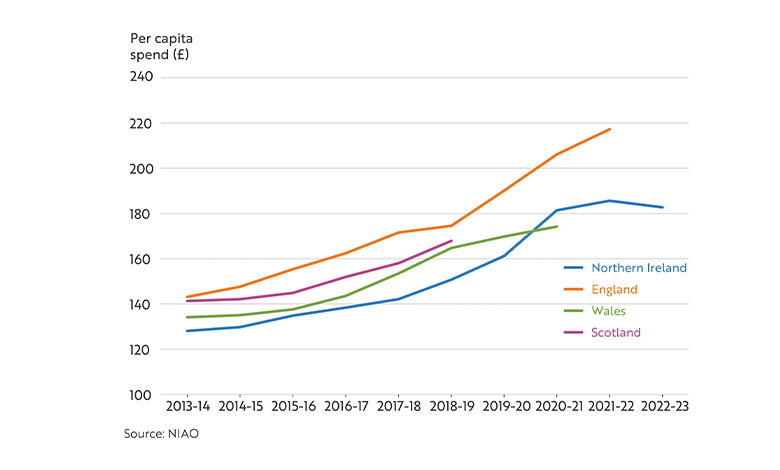
Investment per capita in general practice in Northern Ireland has traditionally been lower than the rest of the UK and as a result, GP earnings in Northern Ireland have been lower than England and Scotland, and on par with Wales.
Service delivery by general practitioners has been impacted by growing waiting lists in secondary care and an ageing population. In 2022/23 funding per patient for general practice saw a 7 per cent real-time cut compared to the previous year.
One of the recognised challenges for GP practices is the cost of up to £1,000 per day to attract locum doctors. The report by the Audit Office highlights that while paying such rates may help immediately stabilise practices “it may have distorted the locum GP market, resulting in higher costs being incurred more generally.”
While acknowledging efforts by the Department of Health to address some of the workforce challenges facing GP practices, the Audit Office has highlighted the absence of a specific workforce strategy for general practice, or specific targets for the growth of the GP workforce, as exists in England and Scotland.
Among the Comptroller and Auditor General’s recommendations is the need for a workforce plan for general practice and refresh the retention schemes that are currently in place.
GP investment in UK regions
Investment in general practice in Northern Ireland has been traditionally lower than elsewhere in the United Kingdom.
Multi-disciplinary teams
Compounding pressures on primary care is a long-standing failure to transform healthcare delivery in Northern Ireland. While incremental changes have taken place since the publication of the Bengoa report in 2016, financial and political instability have stymied successive transformation programmes.
This is evident in the “limited progress” identified by the Audit Office in relation to the rollout of multidisciplinary teams (MDTs) within primary care settings. Considered a key component of health and social care service transformation, MDTs were launched in September 2018 with an incremental five-year roll out plan across all 17 GP Federation areas. However, MDTs have been fully introduced in just one area to date, with partial introduction in a further seven areas.
The Audit Office finds that just 8 per cent of registered patients have access to a full range of MTD roles, and points to a lack of available and qualified staff as a key constraint.
Commenting on the report’s findings, the Comptroller and Auditor General, Dorinnia Carville, says: “Measures taken to date have largely been short-term, which can be costly for public finances. At the same time, progress on delivering more meaningful transformation, such as the planned rollout of multidisciplinary teams to work alongside GPs, has been significantly delayed.
“Ultimately this results in patients not receiving the timely support and access to treatments that they need.
“It is important to note that there are no quick or easy solutions. What is essential now is the development of sustainable long-term plans to address the significant challenges facing GP services in Northern Ireland.”





