The health service under Covid-19

As of 30 June 2020, over 311,000 people are on waiting lists for a first consultant-led appointment in Northern Ireland; a figure that represents 17 per cent of the population. Covid-19 has served to exacerbate Northern Ireland’s already excessive waiting times for health and social care services. agendaNi examines the figures published by the Department of Health and NISRA.
Health Minister Robin Swann warns: “A necessary focus on dealing with the virus created a virtual lockdown of normal health and social care services. This has had an inevitable and serious impact on waiting lists that were already far beyond being unacceptable.”
Outpatient waiting times
The ministerial target for outpatient waiting times in 2020/2021 indicates that by March 2021, at least 50 per cent of patients should wait no longer than nine weeks for a first outpatient appointment and that no patient should wait longer than 52 weeks.
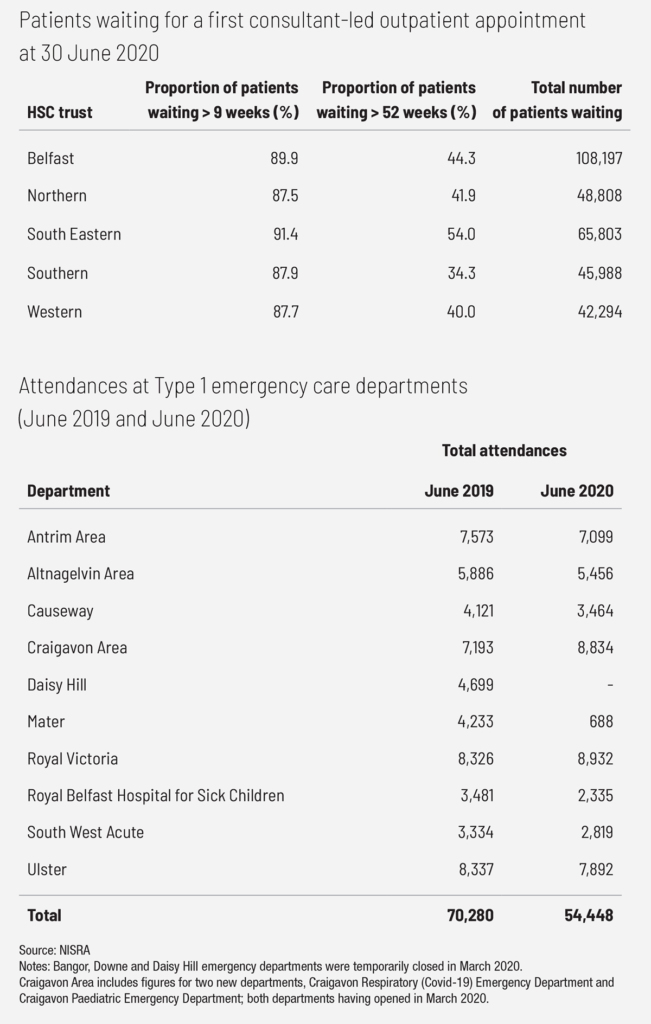
At 30 June 2020, a total of 311,090 patients were waiting for their first consultant-led appointment, an increase of 3.9 per cent (11,654) at 30 June 2019. In June 2020, almost 90 per cent (277,704) of patients were waiting more than nine weeks and over 43 per cent (136,666) of patients were waiting more than 52 weeks for a first consultant-led outpatient appointment.
In Q2 of 2020 (ending June 2020), there were 41,500 attendances for a first outpatient appointment. This is 78,161 (65.3 per cent) fewer attendances than in Q2 2019 when there were 119,661 attendances.
Inpatient waiting times
The ministerial target for inpatient and day case waiting times in 2020/2021 indicates that by March 2021, 55 per cent of patients should wait no longer than 13 weeks for treatment and that no patient should wait longer than 52 weeks.
At 30 June 2020, a total of 97,243 patients were awaiting admittance to hospitals, an increase of 11.3 per cent (9,890) at 30 June 2019. In June 2020, almost 90 per cent (86,337) of patients were waiting more than 13 weeks and almost 40 per cent (38,354) were waiting in excess of 52 weeks for admission for inpatient or day case treatment.
In Q2 2020 (ending June 2020), 14,654 patients were admitted for inpatient day case treatment. This is 30,534 (67.6 per cent) fewer admissions for treatment than in Q2 2019 when there were 45,188 admissions for treatment.
Diagnostic service waiting times
The draft ministerial target for diagnostic waiting times in 2020/2021 indicates that by March 2021, 75 per cent of patients should wait no longer than nine weeks and no patient should wait longer than 26 weeks.
At 30 June 2020, a total of 149,403 patients were waiting for a diagnostic service, an increase of 7.8 per cent (10,756) at 30 June 2019. In June 2020, almost three-quarters (110,225) of patients were waiting more than nine weeks for a diagnostic test and over one-third (52,393) were waiting in excess of 26 weeks for a diagnostic test.
Diagnostic reporting waiting times
The draft ministerial target for diagnostic waiting times in 2020/2021 indicates that by March 2021, all urgent diagnostic tests should be reported on within two days of the test being undertaken.
In Q2 2020 (ending June 2020), 235,019 diagnostic tests were reported on and dispatched to the referring clinician across hospitals in Northern Ireland. This is 192,566 (45 per cent) fewer instances than in Q2 2019 when 427,585 diagnostic tests were reported on and dispatched.
Reaction
Royal College of General Practitioners Northern Ireland Chair Laurence Dorman emphasises that waiting lists “have been completely unacceptable for years” and that the Covid-19 pandemic has “made a bad situation worse”.
“The current waiting list figures paint a very bleak picture, and behind each number is a person whose quality of life is being badly affected… Frequently patients feel they have no choice but to explore private care options, however, this is not an option for everyone. All patients must have equal access to the treatment they need through our National Health Service. We cannot see health inequalities in Northern Ireland widen even further as a result of our appalling waiting lists,” he said.
Likewise, speaking with BBC NI, Gavan McAlinden, an orthopaedic surgeon from the Royal College of Surgeons criticised the slow return to normal operating, emphasising: “While we will always try to minimise the risk to ourselves and to our patients, we are keen to resume, to a much greater extent, our elective service… From my point of view, as a surgeon and as an advocate for patients, I would be keen to see things move along as fast as they possibly can.”
From December 2019 into January 2020, for the first time in its history, the Royal College of Nursing (RCN) undertook strike action. Alongside hospital staff and other healthcare workers, nurses staged a series of strikes over pay inequality, unsafe staffing levels and unprecedented pressures on the health service. Prior to the strikes, Director of the RCN in Northern Ireland Pat Cullen stated: “Being in need of health care in Northern Ireland is a total dread for our population knowing they will sit on year-on-year waiting lists. It’s certainly not easy for nurses knowing patients cannot get care they are entitled to.” In February, nurses accepted a deal proposed by Health Minister Swann which promised pay rises and increased student nursing capacity.
In the context of Covid-19, Cullen subsequently warns: “As we come out of this pandemic, we need to ensure that staff are rewarded and valued properly moving forward. We also need to ensure that the issues that were on the table, such as the promise of legislation for safe nurse staffing are not forgotten about.
“If this pandemic has shown us anything, it is that we cannot compromise on the need to ensure we have the right number of nurses and other health care staff. It is impossible to deliver services without them.”
The Health Minister stated: “Infection control measures are going to be with us for some time and inevitably, despite our rebuilding efforts, this will have an adverse impact on waiting times for procedures,” adding: “These constraints are certainly not unique to Northern Ireland.”
Emergency waiting times
Conversely, emergency care waiting time statistics for Northern Ireland during June 2020 indicate a significant reduction in attendances when compared with the same period in 2019. In June 2020, there was a total of 54,448 attendances at emergency care departments compared with 70,280 attendances in June 2019. This means that total attendances decreased by 22.5 per cent (15,832) from one year to the next. The number of emergency admissions to hospitals from emergency departments also decreased by 16.6 per cent (2,065) from 12,425 in June 2019 to 10,360 in June 2020. However, this decrease was not universal and both Craigavon Area and the Royal Victoria emergency departments recorded increases in attendances of 22.8 per cent (1,641) and 7.3 per cent (606) respectively.
Aimed at rebuilding health and social care services in Northern Ireland, the Strategic Framework for Rebuilding Health and Social Care Services was published in June 2020, with plans reviewed on a quarterly basis. Each of the six health trusts have published local plans for the immediate work being undertaken to scale up services.
However, this rebuilding will be constrained by the ongoing threat of a Covid-19 resurgence. The Health Minister warns: “We are facing into a very difficult winter for an already fragile health service.”